Useful information
Prime News delivers timely, accurate news and insights on global events, politics, business, and technology
Useful information
Prime News delivers timely, accurate news and insights on global events, politics, business, and technology
Every year, about 185,000 people in the United States are subjected to amputation. Almost half of them are due to the injured blood vessels that cut the circulation to a limb. Surgeons can transplant an intact vein from another place in a patient’s body to avoid amputation, but not all have an adequate vein to harvest.
A new advance in fabric engineering could help. In December, the food and medication administration approved a Bioingenated blood vessel To treat vascular trauma. Made by the Biotechnology Company based in Norte Humacyte, it is designed to restore blood flow in patients with traumatic lesions, such as shots, car accidents, industrial accidents or combat.
“Some patients are so injured that they have no available veins,” says Laura Niklason, founder and CEO of Humacyte. Even when a patient has one usable, a vein is often not a good replacement for an artery. “Your veins are very thin. They are small weak structures, and your arteries are very strong, ”she says.
Niklason was interested for the first time in the idea of growing blood vessels in the 1990s, when he was training to be a medical at the Massachusetts General Hospital. She remembers having observed a patient under a cardiac bypass, which implies the use of a healthy vessel to redirect blood flow around a blocked coronary artery. The surgeon opened both legs, arms and finally the stomach, in search of an adequate blood vessel to use. “It was really really barbarian,” says Niklason. She thought there had to be a better way.
It began with the blood vessels in the laboratory of only a few cells collected from pork arteries. When he transplanted them to the animal, they worked as the real.
After those first experiments, it was a long road to an FDA approved for humans. Niklason and his team spent more than a decade isolating the cells of the blood vessels of human organs and tissue donors. They tested cells of more than 700 donors and discovered that those of five of those donors were the most efficient to cultivate and expand in the laboratory. Niklason says that Humacyte now has enough bench cells of these five donors to make between 500,000 and one million blood vessels designed.
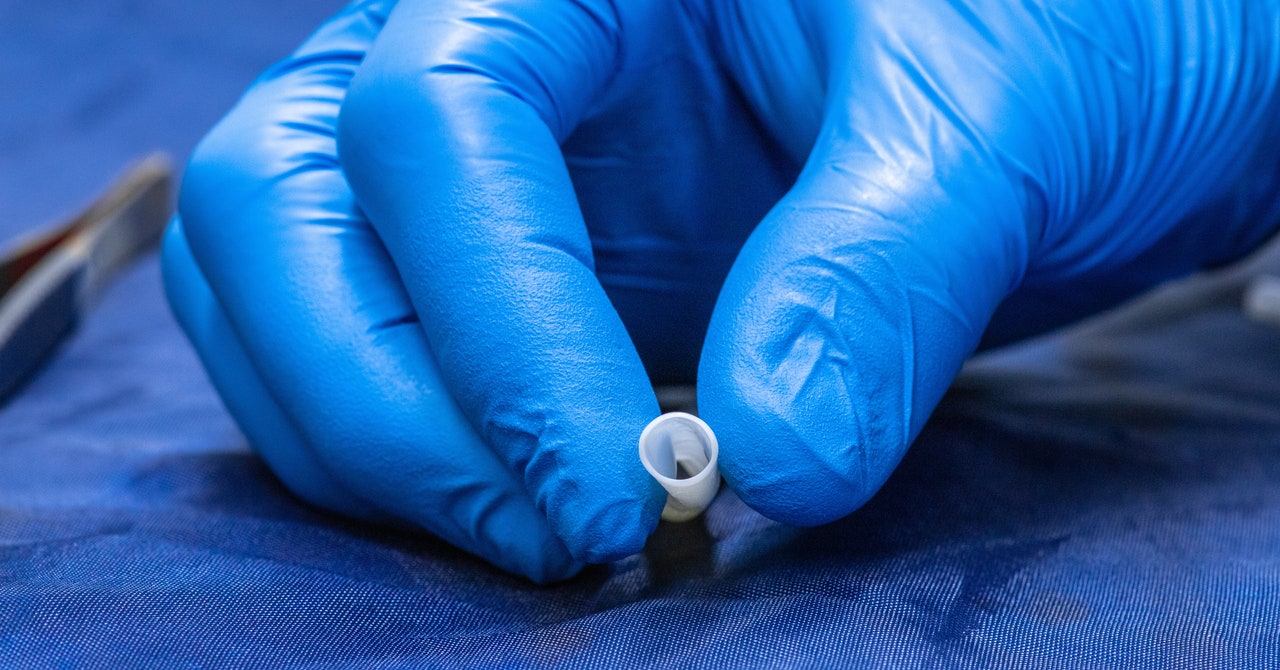
Currently, the company manufactures ships in lots of 200, using degrable polymer scaffolding designed as they have 42 centimeters long and 6 millimeters thick. The scaffolding are placed in individual bags and are sown with millions of donor cells. The bags then enter a school -sized incubator to soak up in a nutrient bath for two months. While the tissue grows, secret collagen and other proteins that provide structural support. Finally, the polymer scaffold dissolves and the cells are removed with a special solution. What remains is the “de -elularized” flexible fabric in the form of blood vessels. Because it does not contain living human cells, it will not cause rejection when it will be implemented in a patient.
“People have been trying to create a tubular material like this for a long time,” says Anton Sidawy, elected president of the American Surgeon and Vascular Surgeon at the George Washington University Center, which is not involved with Humacyte.